Here in the Southeast many patients have a long history of smoking most of their lives. In at least 80% of lung cancer or bronchogenic carcinoma cases in our part of the country, a direct link can be made to smoking and tobacco use. Usually the typical patient presents to his physician with symptoms of shortness of breath, cough, morning sputum production or an occasional episode of coughing up blood. At other times, the patient may be asymptomatic and deny any significant pulmonary symptoms.
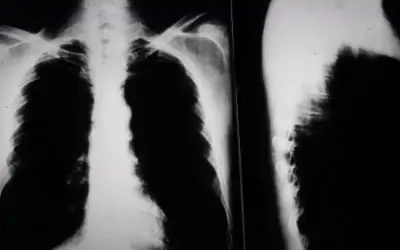
More commonly, the patient has smoked 1-2 packs per day for many years and despite the efforts of his family and doctor, has been unable to stop smoking. Other times, a routine chest x-ray shows a solitary pulmonary nodule or lump in the lung which appears to be abnormal. When a nodule is found, it presents both a diagnostic and a therapeutic dilemma as well as a chance to "cure" early lung cancer.
Most solitary lesions are between 1 and 4 cm in diameter and are well circumscribed with normal lung surrounding the lesion. There is usually no evidence of any other abnormality on the chest x-ray and the lesion itself appears round in shape. In some cases, if old x-rays can be found to compare with the current films, and if the lesion is unchanged for more than 2 years, we can say that it is most likely a benign scar or an area of healed pneumonia. Unfortunately, this is rarely the case with most patients who smoke.
The first step in the workup of a solitary lung lesion that your physician may recommend is to obtain a CAT scan of the chest and lungs and mediastinum (the area between the lungs). The CAT scan generates a scan density number of the lesion measured in Hounsfield units. The higher the number, the more often the lesion is benign. Very high numbers and very low numbers are pretty reliable, but the mid range is still in question. Therefore, in these patients, a second test called a CT directed needle biopsy of the lesion is performed.
This test works the best when the lesion is near the edge of the lung and is more risky to the patient if the lesion is close to a major artery, airway, or the heart. If the lesion is close to the edge of the lung, a needle biopsy may be the safest and most cost effective route toward the final diagnosis. This technique is not without its own complication rate and carries a 15% chance of a pneumothorax (collapsing the lung) from the test even when performed properly.
Another test often recommended by thoracic surgeons is called a fiberoptic bronchoscopy. A small tube with a light on the end is introduced down a patient's airway and into the lung to look at the air passages for signs of tumor. The patient is sedated, but not put to sleep for the test. The test takes about 10 minutes and may provide alot of information about the internal anatomy of the lung. If the lesion can be seen, it can be biopsied, brushed with a small brush for cells, or washed with saline for cytology examination. These specimens are sent for cultures to rule out tuberculosis, fungus, bacteria and a look under the microscope to search for cancer.
Another new tool in the search for cancer is called thoracoscopy. This test has been available since 1993. A small TV camera is placed into the patient's chest via a small incision and if the lesion is near the edge of the lung, it can be excised or wedged out with a stapling device. The nodule is then sent to the pathologist for evaluation under the microscope and a diagnosis is then made. If the lesion is benign, the work-up is complete and the patient can resume his normal activity schedule in about a week.
If the lesion is found to be tumor, then a metastatic screening process must be carried out to look for tumor in other areas of the body. Patients with neurological symptoms should have a CAT scan of the brain to look for brain METs. Patients with this finding are usually offered radiation treatments to both the lung and the brain and not surgery. Patients with bone pain undergo bone scans to look for involvement in the skeleton. A program of nonsurgical management would then be started involving both radiation and chemotherapy.
If the original CAT scan of the chest showed enlarged lymph nodes between the lungs in the area called the mediastinum, then another test called a mediastinoscopy is recommended. For this test, the patient is put to sleep and a small incision is made at the base of the neck. A tube with a light on the end is advanced down to the area which contains the lymph nodes and the lymph nodes are removed. If tumor is found, the patient may be inoperable.
Lastly, a test called pulmonary function studies or breathing studies is recommended to assess the over all capacity of the lung. It also helps the surgeon determine how much lung could safely be removed if surgery is the best option to treat the tumor. Once the work-up is completed and the patient seems to be an operative candidate, then plans are made for surgery. The surgery itself involves removal of the area of the lung which contains the tumor or the area where the nodule was originally located. The post operative recovery time is about 6 weeks, but in my experience it can be much longer depending on the age of the patient and his or her ability to stop smoking after surgery.
Recommendations:
1) If you have pulmonary symptoms get a chest x-ray.
2) If a lesion is found in your lung, have your doctor proceed down the work-up algorithm outlined above.
3) If surgery is recommended, once the diagnosis is established surgery remains the best chance for cure. Lung cancer cures are directly related to how early the tumor is removed so don't put it off too long.
